
You have been advised to have an upper gastrointestinal endoscopy to help find the cause of your symptoms. The test is sometimes called a Gastroscopy or simply an endoscopy. This is a procedure using a special tube to look at the lining of your gullet (oesophagus), your stomach and first part of your intestine (duodenum).
We want to make you as comfortable as possible during your stay. We have written this information to answer the commonly asked questions about gastroscopy. If you have any questions, or if there is anything that you do not understand, please ask when you attend for the gastroscopy.
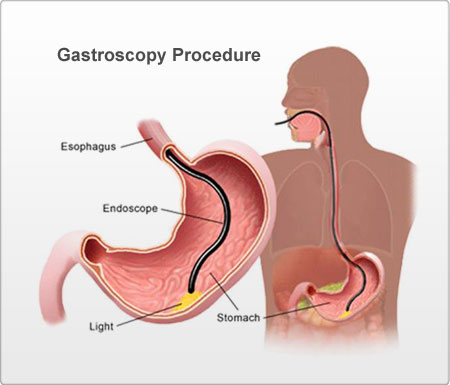
The doctor can study the mucous membranes of the stomach from top to bottom, see irritations, wounds, or tumours. Gastroscopy is effective, and has now replaced the use of x-rays in many cases. It helps the doctor see any abnormalities in the gullet, the stomach and the duodenum. It is precise and safe.
Patients are often given a gastroscopic examination because of their indigestion symptoms, which can usually be treated with medication.
Occasionally, the cause of indigestion is an ulcer and it is known that many ulcers are due to bacterial infection in the stomach
A very small number of patients with indigestion will turn out to have cancer and, again, the diagnosis can be made accurately by biopsy. Further investigation can then be planned to ensure the most effective treatment.
A gastroscopy is carried out with a local anaesthetic throat spray and/or sedation. A gastroscope is a thin, flexible tube with a bright light at the end. It is passed through your mouth, down your gullet and into your stomach. During the test, photographs may be taken.
Sometimes a small amount of tissue (biopsy) may need to be taken from a particular area for examination by the laboratory. The tissue is removed using tiny forceps passed through the gastroscope. You may feel a tugging sensation.
You will be asked to lie on your left side on a trolley and made as comfortable as possible. A nurse will stay with you throughout the test. A probe will be placed on your finger to monitor your pulse during the test. If you have chosen sedation it will be given at this point. To protect your teeth (and the endoscope) a small plastic mouth guard will be placed between your teeth. This will not interfere with your breathing. The gastroscopy takes around 5 – 10 minutes to complete. When the examination is finished, the endoscope is removed easily, causing little discomfort.
If you have had sedation you will need time for the sedation to wear off. If you have had local anaesthetic throat spray, you will not be able to eat or drink for 2 hours after the examination, or until the swallowing reflexes are back to normal. After this you can eat and drink normally. The back of your throat may feel sore for the rest of the day. You may also feel bloated if some of the air has remained in your stomach. Both these discomforts will pass and need no medication.
This is a safe procedure. Complications such as perforation (tear in the wall of the gullet or stomach) and bleeding can occur, but are rare. You will be monitored closely throughout the examination and if there is any cause for concern, the test will be stopped immediately.
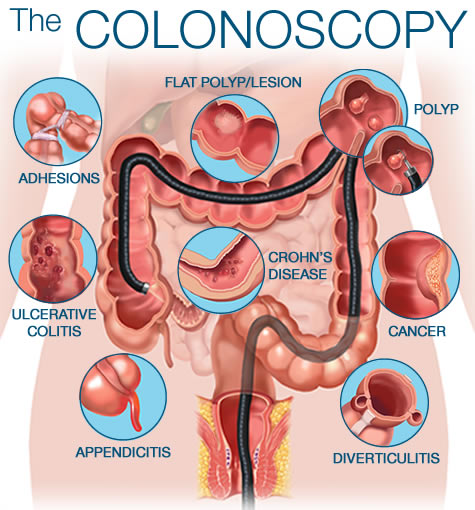
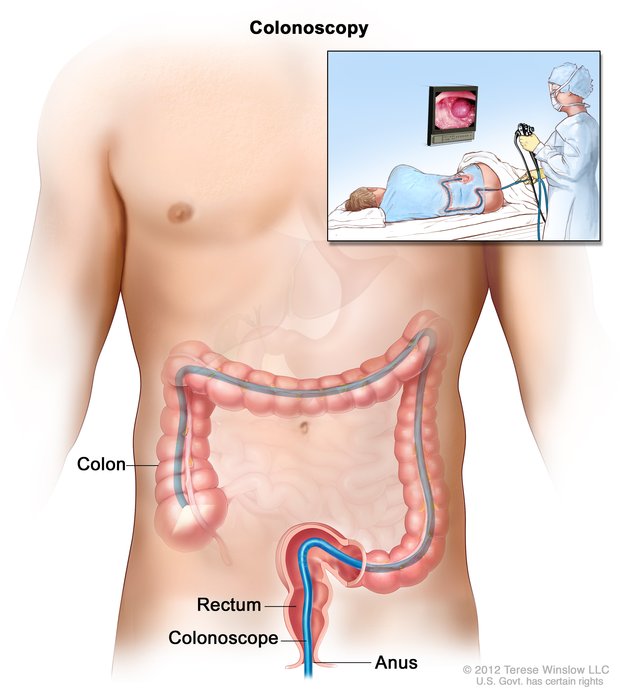
Colonoscopy is a test where your doctor looks into your colon. The colon is sometimes called the large intestine or the large bowel. This procedure allows the doctor to look inside your entire large intestine, from the lowest part, the rectum, all the way up through the colon to the lower end of the small intestine. The procedure is used to diagnose the causes of unexplained changes in bowel habits. It is also used to look for polyps and early signs of cancer in the colon and rectum.
During the procedure, the doctor uses a colonoscopy which is a thin, flexible telescope. It is about as thick as your little finger. The colonoscope is passed through the anus and into the colon. It can the be pushed all the way around the colon as far as the caecum (where the small and large intestine meet).
During the procedure, the doctor uses a colonoscopy which is a thin, flexible telescope. It is about as thick as your little finger. The colonoscope is passed through the anus and into the colon. It can the be pushed all the way around the colon as far as the caecum (where the small and large intestine meet).
Colonoscopy is usually done as an out-patient or day case. Before your procedure you will be asked to change into a hospital gown and lie on your left side with you legs in a curled position. The procedure itself takes around 20-30 minutes. A colonoscopy does not hurt, but it can be a little uncomfortable, particularly when the scope is first passed into the anus.
You may be experiencing a change in your normal bowel habit and/or abdominal pain which needs to be investigated. You may be bleeding through your back passage or you may have anaemia (low blood count), for which your doctor needs to find the cause.
We may diagnose diverticular disease (small pockets that are created in the lining of the colon). This can be controlled with diet and mediction.
The diagnosis may be haemorrhoids (piles), which can sometimes be treated during colonoscopy, depending on severity.
A colonoscopy is sometimes carried out to see if you have a polyp (innocent growth) that can be removed during colonoscopy. If polyps are found you may need to have a repeat colonoscopy at a later date to check for recurrence.
Sometimes a colonoscopy is carried out to see if you have a tumour, following which you may need to have an operation.
Sometimes a colonoscopy is carried out to see if you have a tumour, following which you may need to have an operation.
Tumours of the colon can run in families, therefore, if this is known to be the case, you may be advised to have a colonoscopy on a regular basis. We do this because colon tumours are curable if caught early.
To allow a clear view, whole colon must be completely empty of waste material. It is essential that you drink the 3 sachets of fleet that the doctor prescribes for you and to drink plenty of clear fluids. You will be provided with an information sheet on how to take the medicine.
Most colonoscopies are done without any problems. If you have had a sedatve you may feel tired or sleepy for several hours afterwards. You may pass a small amount of blood from your anus if a biopsy was taken, or a polyp removed, Occasionally the colonoscope may cause damage to the colon. This may cause bleeding, infection and rarely, perforation. If any of the following occur within 48 hours after a colonoscopy, it is important that you consult your doctor immediately:
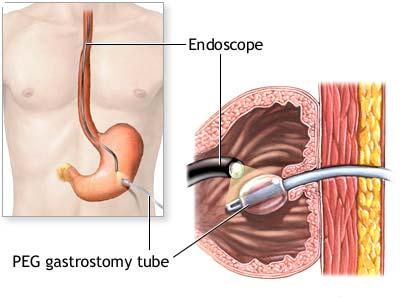
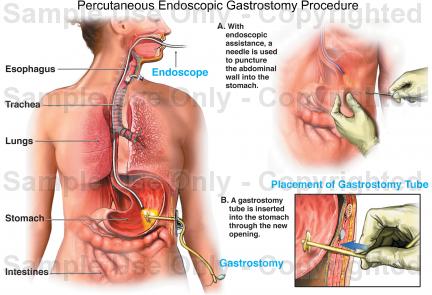
Percutaneous endoscopic gastrostomy (PEG) is a surgical procedure for placing a feeding tube without having to perform an open operation on the abdomen (laparotomy). A gastrostomy (a surgical opening into the stomach) is made percutaneously (through the skin) using an endoscope (a flexible, lighted instrument) to determine where to place the feeding tube in the stomach and secure it in place.
The aim of PEG is to feed those who cannot swallow. Irrespective of the age of the patient or their medical condition, the purpose of PEG is to provide fluids and nutrition directly into the stomach.
PEG is done by a doctor. The doctor may be a general surgeon, an otolaryngologist (ENT specialist), a gastroenterologist (GI specialist), etc.
Local anesthesia (usually lidocaine or another spray) is used to anesthetize the throat. An endoscope (a flexible, lighted instrument) is passed through the mouth, throat and esophagus to the stomach. The doctor then makes a small incision (cut) in the skin of the abdomen and pushes an intravenous cannula (an IV tube) through the skin into the stomach and sutures (ties) it in place.
The patient can usually go home the same day or the next morning.
PEG takes less time, carries less risk and costs less than a classic surgical gastrostomy which requires opening the abdomen. Therefore, when feasible, PEG is preferable to a classic gastrostomy.